PREMIUM
LAURA TARDÓN
Madrid
Saturday, 2 January 2021 - 22:09
Share on Facebook
Share on Twitter
Send by email
See 1 comment
Live.
Coronavirus news
Sanitary.
Those who never stop fighting the coronavirus
One year later.
The rebirth and wounds of the epicenter of the pandemic
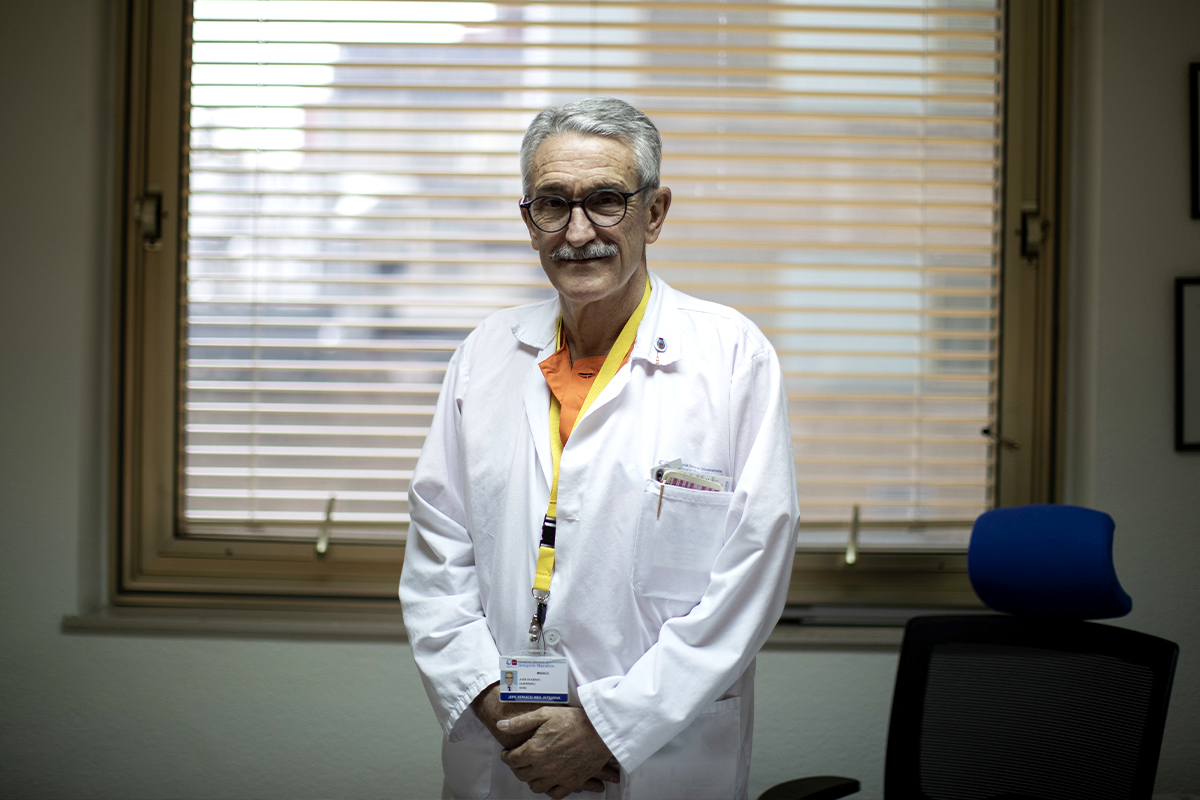
José Eugenio Guerrero was the voice of all the health workers in Spain when he received the Princess of Asturias Award last October and is head of the ICU at one of the largest hospitals in Spain, the Gregorio Marañón in Madrid.
After months of battles against the coronavirus, he dedicated the tribute to his colleagues, "men and women who dedicated their lives to taking care of other lives and who took their generosity and commitment to the extreme."
In honor of his memory.
"We will never forget" them, he said, as well as this health crisis, "the worst that the world has faced in the 21st century."
In his 40 years as an intensivist doctor, he claims not to have experienced "anything like this terrible pandemic."
Neither the 11M nor the rape nor the AIDS nor the Flu A ...
It has been a year of great losses.
Twelve months after the first cases were reported in the Chinese city of Wugan, how do you remember those days in Spain? At first, we saw respiratory disease that we classified as influenza pneumonia.
Until March, everything was sensations and already in the first week of that month, we decided to go down to the emergency room with protection and gloves because we were not at all clear how the disease was going to evolve.
We lived it with restlessness because we did not know very well what was waiting for us.
Soon, our doubts were removed to know that it was the most terrible disease that we had experienced or, at least, that I remembered in the more than 40 years that I have been an intensivist.It is true that we saw terrible X-rays with bilateral infiltrates and very sick but we never expected that in a matter of days, what were two cases in the ICU would become 50. The hospitals were overcrowded.
How did you deal with this avalanche of cases in the ICU of the hospital where you work?
What resources did they lack? In the first wave, we lacked everything, even time to see the sick.
We would leave in the late afternoon / evening and come back again at 7.30 the next morning and still, we had the feeling that we had not done everything we would have liked.
There was a lack of means, time, everything ... And we are talking about a hospital that was able to go from 18 beds in ICU to have 120. See 120 ICU patients and be able to have 120 spaces, respirators and qualified personnel to be able to see to this type of patient ... All services were overturned.
It is a huge job.
Every day 10 more beds had to be opened for the sick.
To what extent did fear affect you? With the overflow of cases in front of us, there was not much room for fear, except for people with sick or immunosuppressed children or relatives who did experience it with anguish because they knew that if they were carrying covid home, you could end up with your father, mother or a child with compromised diseases.
From the psychological point of view, how is this situation affecting you? Intensivists are educated from day one to see the misfortunes of society, but it is true that the intensity of this pandemic has no comparison with anything.
We have suffered the loss of tremendously loved colleagues and we have taken home the cases in which we have made decisions that on other occasions we would have made faster.
In the intensivist team, have there been many casualties due to covid? I have not happened.
We have saved very little.
Approximately 80% have had covid in other medical services.
Fortunately, in the intensive care unit, we were gradually discharged.
Immersed now in this second wave of SARS-CoV-2, what differences do you observe compared to the first months? In the first wave, everyone endured going to the hospital.
People arrived very badly and immediately went from the emergency room to the ICU because they needed respiratory assistance.
In the second wave, patients have arrived earlier and can be better managed.
We can put measures to protect the evolution of the disease, with the use of corticosteroids and some treatment that is associated to avoid superinfections, although there is still no treatment for Covid.
Also, in the first wave, only covid was seen, nobody came to the hospital for other reasons.
Now we do see other pathologies.
And as for the patient's profile, has it changed? People are younger.
In this second wave, we have seen fewer people aged 70 and over than in the first few months.
We see more cases between 45 and 65 years of age than before. There was even talk of selecting patients for the use of respirators, since there were not enough.
How was this experienced in the UVI of Gregorio Marañón?
What a doctor wants is to have the means and treat all the sick even if he had to leave at four in the morning.
We would leave late at night, but it is also true that we did not leave with the satisfaction with which intensivists usually go home from having done things the way we think they should be done.
We would leave work for the next day due to lack of everything, means, space ... A pandemic of these characteristics is not controllable, neither at a health nor political level.
Suddenly hundreds of patients entered through the emergency room with the same pathology. At Gregorio Marañón, we have not really had problems with the availability of respirators.
How do you think these days will affect the evolution of infections in Spain? We all fear the third wave.
I do not understand epidemiology and as an intensivist I cannot speak, but as José Eugenio Guerrero, personally, I would suspend Christmas and celebrate it later.
Now that we see the vaccine close and we can possibly control the pandemic in a short time, I think we have to make the effort to suffer this month so that in March, April or May we are released.
As a common citizen, I think we should try not to add more deaths and avoid contagion.
What role do you give to vaccines? I have great faith in them and in their role to finally control this situation. Remembering, for example, the applause at 8:00 p.m., do you think that this great crisis has made the population aware of the relevance of the health system and its workers? People during that time felt really represented, happy with health as such, but I think that later on we all forget what has happened.
I understand that if you have a tumor and have not operated for three months, you lose your affection for health because of that wait.
It seems to me that he is human.
From the point of view of healing, what have we learned? That pain and suffering unite.
That there really are no healings but a unique healing.
When it was necessary, the public and private joined forces and was exemplary.
Nobody talked about an A or C bed. What lesson should we not forget for the proper functioning and response of health? A pandemic is intractable, when suddenly so many patients come from the same pathology, it is intractable.
We must be sufficiently aware that this can happen and the better health we have, the more number of beds and the better equipped we are, the better the answer will be and the easier it will be to deal with such terrifying situations.
José Eugenio Guerrero.ALBERTO DI LOLLI
According to the criteria of The Trust Project
Know more
Science and Health
Coronavirus
Covid 19
HealthCovid-19, the failure of the yo-yo strategy to control the pandemic
Mass vaccination in the UK gives priority to those over 80
Coronavirus The Government announces that the Christmas Plan is maintained but leaves the strictest limitations in the hands of the CCAA
See links of interest
Check Christmas Lottery
Check Child Lottery
Tottenham Hotspur - Leeds United
Villarreal - Raise
Fuenlabrada - Leganés
1. FC Cologne - FC Augsburg
Real Madrid - Celta de Vigo, live