For the first time in the world, a patient's heart begins to regenerate after suffering a heart attack thanks to a great bioengineering work. It is a bioimplant of umbilical cord stem cells. An unprecedented success of Spanish science. The results are very exciting and encouraging. Six months after going through the operating room (last May), the 70-year-old man " has gone from practically not leaving home and drowning in small efforts to come to the clinic on foot, " explains Antoni Bayés-Genís enthusiastically , responsible for the cardiovascular disease research team (ICREC) of the Germans Trias Hospital in Barcelona.
"As the patient himself acknowledges, already 10 years ago, his life expectancy was very short and with day-to-day limitations," Bayés-Genís tells this newspaper. The problem: heart failure. When a myocardial infarction occurs, the heart loses strength to beat due to the death of the cells of the injured area, which have stopped receiving blood from the coronary arteries. That is, part of this organ is necrotic or dead and, "to this day, there is no possible solution in clinical practice."
In recent years, a path began to be seen in mice that had managed to form small blood vessels in the infarcted area and reoxygenate it. Through mesenchymal stem cells from the umbilical cord. Later, the group of this Spanish researcher was able to demonstrate that in pigs there was also the reduction of the scar and the consequent improvement of the cardiac function.
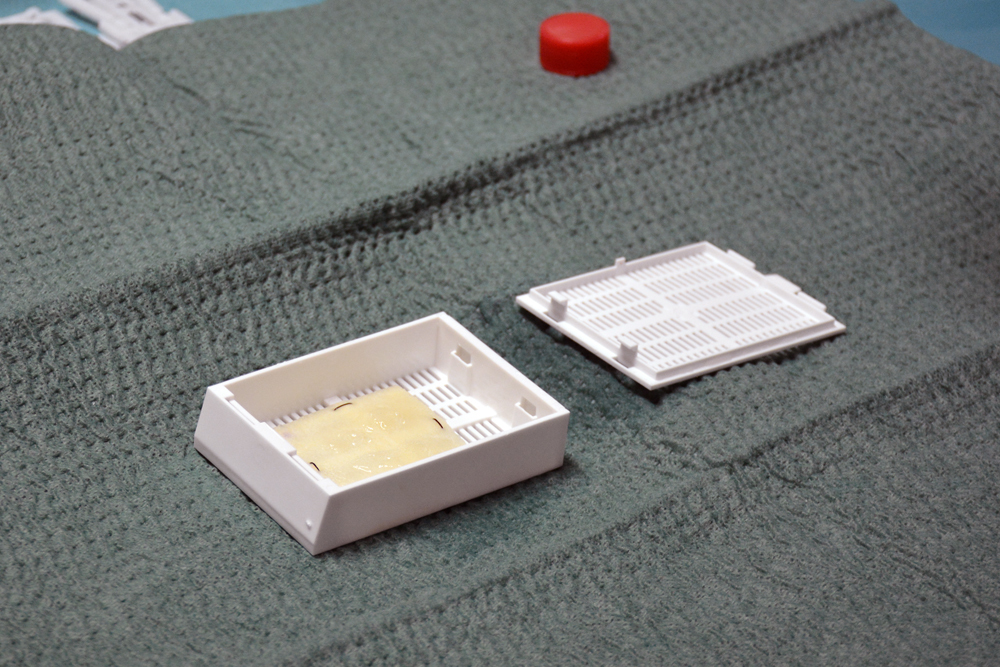
As? From a human pericardium that empties itself of cells and then enriches it with the mesenchymal umbilical cord. Hence its name: PeriCord, which obtained the permission of the Spanish Agency for Medicines and Health Products (AEMPS) at the end of 2018 for use in humans.
With this green light, the jump to the clinic could take place last May at the Germans Trias Hospital. "He was a 70-year-old man, with heart failure and a necrotic heart extension similar to the size of the bioimplant (4x4 centimeters)," Bayés-Genís details. In addition, "it required an open chest operation to place bypass, so taking advantage of this surgery we proceeded to the intervention, which is like a partial heart transplant."
Previously, the bioimplant was prepared with the help of the Bioengineering Institute of Catalonia (IBEC) and in the clean rooms of the Blood and Tissue Bank (BST). The donated human pericardium cells were removed, leaving only the matrix, a flexible, porous and thick membrane where mesenchymal cells of the umbilical cord were then stored. In about six or eight hours, the patch that was to be placed in the patient's heart was ready, taking advantage of the surgery to also put the bypass.
The introduced cells migrate directly to the cardiac tissue, without dispersing. In previous studies, when the cells were administered by injections into the myocardium itself or intravenously, the cells died before benefits were found or were directed towards other different organs. But on board this matrix, the cells travel and act directly at the destination, on the infarcted area .
It is the first time that an operation like this is carried out worldwide and now it's time to track its evolution. According to the MRI, " after three months the scar had been reduced by 10% . A very significant result," says Bayés-Genís.
"This type of cells has been shown to have great plasticity and pluripotence, that is, they have an enormous capacity to become different types of human body cells. In addition, they have important immunomodulatory and anti-inflammatory properties," says the cardiologist.
If it were not for this alternative, Bayés-Genís adds, the patient would have been placed bypass to try to bridge and improve blood circulation, "but if they had not worked, the affected would have required mechanical ventricular assistance and would be a candidate for transplant".
The aim is to prevent transplantation of many infarcts through the regeneration of cardiac tissue with stem cells . At the moment, this option is framed in a clinical trial. Throughout today, a second patient of similar characteristics will undergo the same intervention with the bioimplant. "The idea from now on is to continue the trial in a randomized, prospective and controlled manner until a total of 12" operations with the stem cell patch are made. "If the reparative capacity in humans is confirmed, we could remit usual complications derived from these scars such as heart failure."
This pioneering project has been possible with the support of the Department of Health of the Generalitat of Catalonia, the Carlos III Health Institute and "la Caixa".
According to the criteria of The Trust Project
Know more- Science and Health
Health School menus, to review for the presence of fish with high levels of mercury
Equality Sanity imposes the distinction by sex in the gowns and in the attire of its workforce
Campaign Doctors and nurses are left mustache to make visible the diseases that most affect man