- During a lecture at the Science Festival, you talked about the SARS-CoV-2 virus and the COVID-19 infection. Continuing this topic, I would like to ask what is known about the virus today, how does it develop and mutate?
- We know a lot about the SARS-CoV-2 virus, but not everything.
Nevertheless, we already have important information about what constitutes COVID-19, how to properly treat and prevent severe course of this disease in high-risk patients.
In our life, the virus "officially" appeared at the very end of last year, but there is a lot of evidence that it circulated in the human population in mid-autumn or even at the end of summer 2019.
Even then, there were reports of a fairly large number of patients with symptoms similar to COVID-19.
Of course, since the beginning of the epidemic, the possibility of coronavirus mutations has been discussed.
It must be said here that the continuous change of the genome is inherent in the nature of all viruses.
During the many thousand-fold reproduction of their genetic information, certain "copying errors" occur, leading to the fact that the genetic code is not rewritten "letter by letter".
This also happens so that the virus can escape from the body's immune defenses.
To date, the use of genome-wide analysis has identified at least 100 thousand different variants of the genome of the SARS-CoV-2 virus.
Among them there are more or less stable mutations.
- As a result of the mutation, this virus began to affect people?
- Yes, earlier this virus did not have the ability to infect a person, but as a result of mutation, the S-protein of this virus (the spike protein of the coronavirus, from the English Spike - thorn) was able to attach to certain proteins on the surface of the cells of the human body, that is, the "key" came up to the "castle".
This is how we got this disease and all the related problems.
Moreover, at the very beginning of the epidemic, experimental studies with this virus, which should be carried out on laboratory animals, were simply impossible, since the virus did not infect mice or hamsters.
Computer image of the SARS-CoV-2 virus, whose spines resemble a crown
© NEXU Science Communication / via REUTERS
For this purpose, even transgenic lines of mice were specially bred, which were "humanized", that is, their genome was changed so that their cells began to synthesize "human" versions of the protein, with which the S-protein of the coronavirus binds.
This was necessary in order to study the behavior of the virus and the disease it causes in laboratory animals, to test vaccines and drugs.
- How different are the emerging versions of the coronavirus? Could it be that the vaccines under development will not be able to fight against new modifications of it?
- To date, none of the described mutations fundamentally changed the antigenic presentation of the virus, which is important for the formation of a full-fledged immune response.
Several important conclusions follow from this.
First, the virus is recognized by the human immune system, which destroys it, which leads to the recovery of patients.
And severe cases of the disease are not associated with the activity of the virus, but with an overreaction of the immune system.
Secondly, it provides an extremely low chance of re-infection.
Thirdly, it follows from this that vaccines, the action of which is directed just at this very S-protein of the virus, will be effective.
- Many scientific teams around the world are working on vaccines against COVID-19. What is the difference between them?
- The vaccines under development differ significantly in the technologies used and in the method of inducing an immune response.
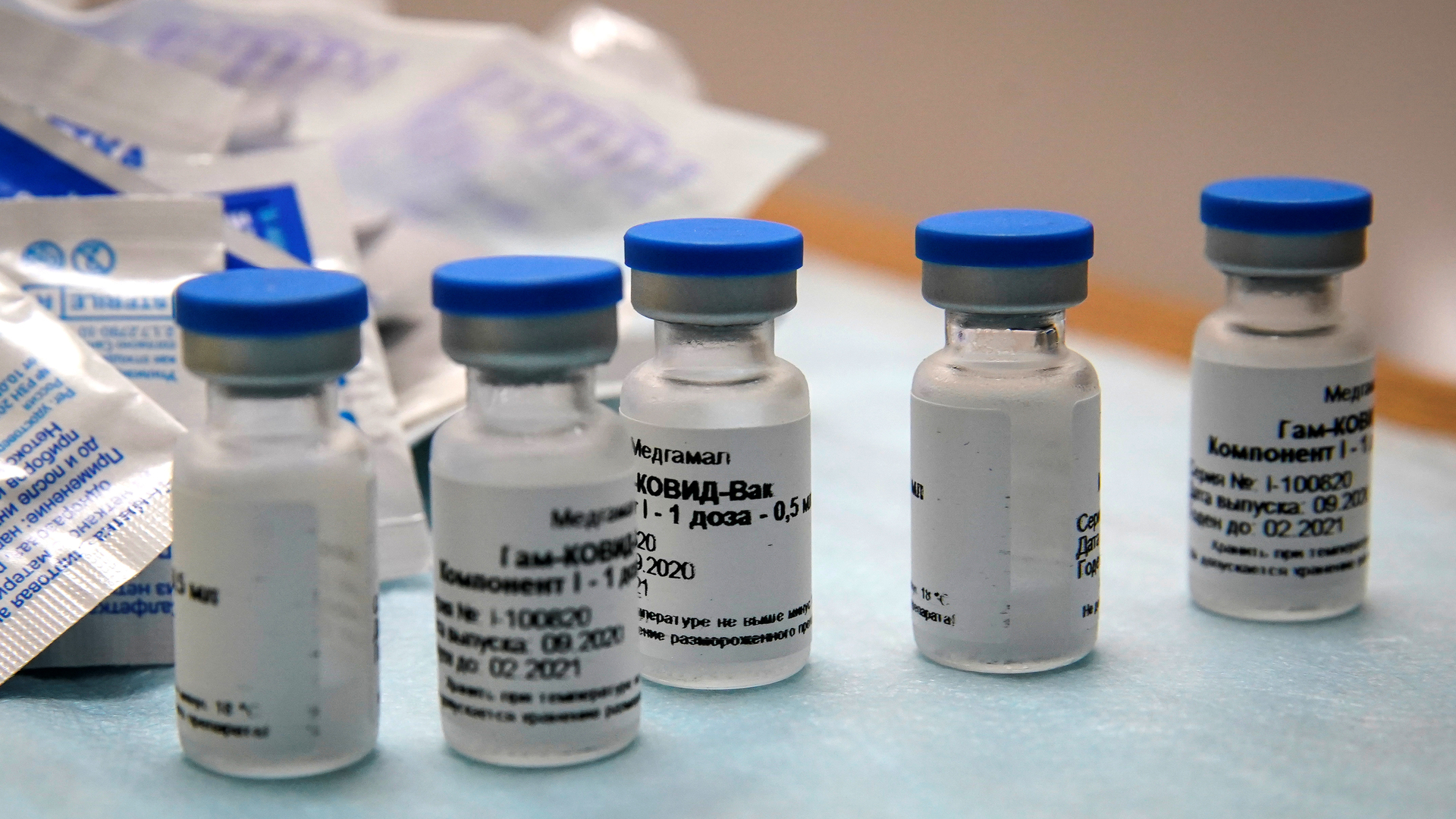
For example, the vaccine of the Institute.
N.F.
Gamaleya "Sputnik V" is based on adenoviral vectors with an "inserted" gene for the S-protein of the coronavirus.
When it enters the human body, an active synthesis of this protein begins, to which an immune response is formed.
And when infected with a "live" virus, its surface proteins will be instantly surrounded and neutralized by already existing antibodies, which makes penetration into cells and replication almost impossible.
Vaccine of the Institute.
N.F.
Gamalei "Sputnik V"
Reuters
© Tatyana Makeyeva
The vaccine, which is being made by the State Research Center "Vector" in Novosibirsk, has a different structure: a synthetic S-protein of the coronavirus is introduced into the body, to which antibodies are synthesized and an immune response is developed.
With this approach, fewer side effects and unwanted reactions are expected, but the immune response will also be weaker.
This approach can be justified when vaccinating the elderly and patients with chronic diseases.
And our colleagues at Oxford University in the UK are developing a vaccine based on the use of chimpanzee adenovirus as a vector, to which humans do not develop an immune response.
Such a vaccine will also be effective.
The Americans are developing a vaccine based on RNA technologies, which has no analogues yet.
Its mechanism of action is based on the introduction of messenger RNA encoding the same S-protein of the coronavirus.
The latter begins to be synthesized in cells and is presented to the immune system as an antigen.
There are many different vaccine technologies, but they all in one way or another involve the synthesis of antibodies to the coronavirus spike protein.
- You have mentioned several domestic and foreign vaccines. Is there an international collaboration of scientists in the fight against a common threat?
- International cooperation continues, despite all the political and even scientific differences.
Vaccines that are being developed in our country will be tested in other countries as well.
The vaccine from Oxford University is being tested in South Africa and Brazil, and is going to be tested in Russia and the United States.
Multicenter transnational research is needed.
A vaccine that will be tested on a Russian population may not work, say, on a Spanish, South African, or South American population.
And vice versa.
This is how the effectiveness is tested on a large number of people, different in racial, ethnic, gender, age composition, and so on.
Vaccines that are being developed in our country will be tested in other countries, and vice versa.
Reuters
© Tatyana Makeyeva
- Still, there are sad numbers, new anti-records for coronavirus statistics in Russia. And it looks like the situation in the world is no better ...
- There is both a medical aspect of the problem and many others.
From a medical point of view, COVID-19, while continuing to remain a serious problem, has ceased to pose a global threat to humanity.
Yes, it is clear that people will become infected, many will be seriously ill, and some, unfortunately, will die.
We are seeing more and more cases in young patients, including children.
But this is a natural process of the development of an infectious disease.
We see a significant, one might say, avalanche-like growth of detected carriers of the SARS-CoV-2 virus in Russia.
Absolutely the same rapid growth as in European countries, in many regions of the United States, in Israel.
What is the reason?
Significant increase in the number of tests performed.
Naturally, the more we test, the more infected people or already sick patients will be detected.
From my point of view, the most important indicator here is mortality.
Not a statistical value reflecting the ratio of deaths to cases, but the number of deaths.
This indicator remained almost unchanged, even decreased after the first outbreak in late spring - early summer.
Now people have returned from vacations, children went to school, students went to colleges and universities, the working season has begun.
Also, social distancing has become much weaker, everyone is tired of restrictive measures.
In addition, now the cold season is coming, when people spend less time on the streets and more indoors.
In the absence of precautions, all this also contributes to an increase in the number of infected.
According to Dr. Matskeplishvili, society's fatigue from restrictive measures also influenced the increase in the number of infected.
globallookpress.com
© Lev Vlasov / Keystone Press Agency
- Virologists also assumed that the virus would weaken, since it was not profitable for it to kill its carrier ...
- There was a lot of talk that the virus seemed to weakened.
In fact, he hasn't changed in any way.
But he shouldn't weaken either.
The virus is weakening as a result of mutations, and this is not at all profitable for us.
- Is there any progress in the treatment of people with severe COVID-19? Are there any new methods of rehabilitation?
- Today this is one of the most important issues.
First, the problem with outpatients who stay at home has not yet been largely resolved.
Their treatment consists in the use of antipyretic drugs, ineffective antiviral drugs and completely ineffective vitamins or microelements.
To our great regret, many of them are completely unreasonably prescribed antibiotics.
Or serious blood thinning drugs.
This, from my point of view, is not true.
Our MSU Medical Center has developed its own COVID-19 treatment protocol based on a pathogenetic approach.
We did not include in it antiviral drugs, antibiotics, and the whole emphasis shifted to the main manifestations of the disease - systemic inflammation and thrombosis.
Also, from the very beginning, patients received therapy that prevents the development of fibrosis, scarring of the lung tissue, and this therapy continued after discharge from the hospital.
- Fibrosis of the lungs is serious, but not the only complication after coronavirus?
- Coronavirus infection has three main target organs.
Lungs, heart and kidneys are affected.
Up to 15% of patients suffer from inflammation of the heart muscle, myocarditis, which can lead to severe arrhythmias or heart failure.
In another 15% of patients, renal function is impaired, and 5% even require renal replacement therapy, that is, hemodialysis.
From the very beginning, anti-fibrotic drugs were prescribed in our treatment protocol, and we have proved their effectiveness in experimental clinical studies.
For 55 days of the operation of the Moscow State University Medical Center in the covid-hospital mode, we treated 424 people.
They were very difficult, we could not save four of them.
The overall mortality rate was 0.94%, which is probably one of the lowest rates in the world.
- Does your protocol involve post-discharge rehabilitation and patient management?
- Yes, the inflammatory process and hyperactivation of the immune system persist for six to eight weeks after discharge, so it is important that a person undergoes a full-fledged rehabilitation and does not have serious long-term consequences.
It should be understood that the severity of the condition of patients in the midst of the disease is not caused by a virus, but by an inadequate reaction of our immune system, which can continue even after the end of treatment in a hospital.
And their future life will depend on the earliest possible rehabilitation program.
- How and when do you think we will defeat the coronavirus?
- Gradually, collective immunity will form when some layer of people gets sick and becomes immune to infection.
Then vaccines will arrive, and a certain part of the population will develop artificial immunity.
And when the virus has no one to infect, it will simply disappear.
I think that in a year we will not even remember about him.