- The third phase of trials of the Sputnik M vaccine for children from 12 to 17 years old has recently started in Moscow. How do children tolerate vaccination easier than adults, or the same?
- The main task of the first and second phases of testing is dose selection.
There is already information on these phases.
First, a completely safe dose for children was selected, this is one-fifth of the adult dose.
Children tolerate this dosage not only well, but very well.
The data are submitted not only to the national regulator, but also to the Independent Data Monitoring Committee.
The results were found to be very convincing, which is why the third phase of the research began.
Children show high immunogenicity, geometric mean, median antibody titers are higher than in adults.
This is not surprising because children have an intact, active immune system and respond very well to vaccinations.
Denis Logunov, Deputy Director of the National Research Center for Epidemiology and Microbiology named after N.F. Gamaleya
RIA News
© Evgeny Odinokov
- Do you plan to launch similar work on a vaccine for children under 12 - preschoolers and primary schoolchildren in the near future? Is it true that it is for the youngest children that the coronavirus can be dangerous?
- The coronavirus can be dangerous for both older children and young children.
Therefore, in fact, a vaccine is being developed.
But you still need to clearly understand that the coronavirus is most dangerous for people over 65-70 years old.
It is in this group that the greatest lethality is noted.
But among children, there are also different cases, they can also be seriously ill.
The vaccine is designed to "close" this part of the population.
- When will the Sputnik M vaccine be available to everyone?
- It no longer depends on the Gamaleya Center.
The center has completely prepared a set of reporting documentation, presented it to the national regulator, to the Ministry of Health.
The regulator, in turn, considers the submitted data in accordance with the established procedure.
As I said, the effectiveness of the vaccine is very good: it gave a minimum of adverse events, even mild ones, with high immunogenicity.
Therefore, we hope that there are no grounds for refusing registration.
As for children of the younger age group, from 6 to 11 years old, the regulation in all countries is arranged in such a way that all research is carried out in stages.
First, the evidence base for the safety and efficacy of the drug is collected on adults, then on children of the older age group, this, respectively, 12-17 years, then 6-11 years, and then the youngest.
You can't skip the stages and start vaccinating two-year-olds right away.
We comply with stringent regulations, both international and Russian.
- You said that the effectiveness of Sputnik V against the delta coronavirus is about 80%. Let's assume that the virus continues to mutate and new strains appear. Are there any tools for predicting the emergence and spread of new strains and how quickly can the required volumes of the updated vaccine be developed and produced?
- An updated vaccine can be developed and produced quickly. Platform vaccines can be very quickly adapted to new options. This is not only our vaccine, but also Pfizer, Moderna, AstraZeneka and Johnson & Johnson vaccines - all of which are platform solutions. In order to timely adapt the vaccine to new strains, there is only one way - monitoring the situation. Monitoring in the country is being carried out, and this is being done at the Gamaleya Center, together with the Moscow Healthcare Department, and at the Influenza Institute, in St. Petersburg, and at the research centers of Rospotrebnadzor. Samples are taken from the population, and circulating strains are constantly monitored. If a new strain with greater pathogenicity, greater transmissibility, greater lethality appears, then the vaccine will need to be updated.This can be done quickly enough - in just a few months.
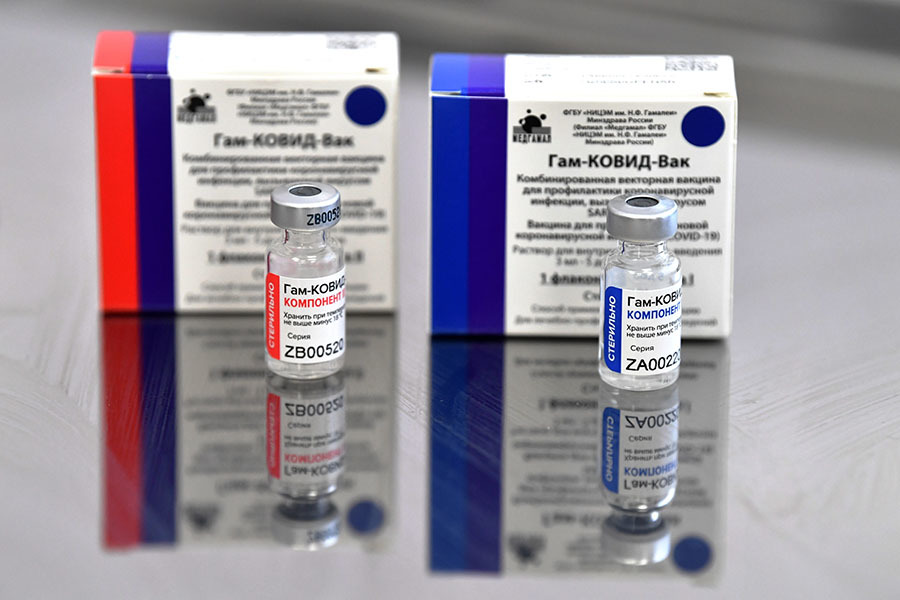
Vaccine against COVID-19 "Sputnik V" ("Gam-COVID-Vac")
RIA News
© Pavel Bednyakov
- Is there a need to update the vaccine for the delta strain? Or is the efficiency that we have now enough?
- This issue is now on the agenda.
We do not exist in a vacuum, but in a vast world where there is experience in the use of vaccines - both in the United States, and in Israel, and in Europe.
Now the strategy of the third vaccination has been chosen, which effectively restores the decrease in immunity to the virus, which is observed by the sixth-eighth month after the first vaccination.
Russia is also following this strategy.
In principle, if the delta strain is stable, it will be possible to consider adapting a vaccine to it.
But now the effectiveness of the vaccine is still higher than the requirements of the WHO.
As you can see, Pfizer and Moderna have yet to release a new vaccine either.
However, in any case, you need to be prepared for such a need.
The Gamaleya Center prepares for this not only mentally, we have obtained all vaccine strains, their safety and effectiveness have been tested on animals.
Inspection lots have been released so that limited clinical trials can be run if necessary.
Vaccine strains are routinely updated and put in the form of a kind of "canned food".
- At the beginning of the use of vaccines (all, not only "Sputnik V"), a lot of hopes were pinned on T-cell immunity, they said that the effect of the vaccine would last for several years or even for life. But in fact, in all countries it turned out that a booster vaccination is needed to ensure a high level of antibodies. Is there any cellular immunity to coronavirus?
-
Cellular immunity to coronavirus exists.
And, naturally, it plays a role in containing the coronavirus infection.
You simply cannot use cellular immunity as a surrogate marker.
(a surrogate marker is a criterion that, in essence, is not the desired outcome of treatment within the framework of the study. -
RT
).
National Research Center for Epidemiology and Microbiology named after
Gamaleys in Moscow
RIA News
© Ramil Sitdikov
To determine the strength of cellular immunity, peripheral blood cannot be used. T cells have such a thing as homing. The cells multiply, are thrown into the bloodstream, then they are seated in the immune lymphoid organs - in the bone marrow, in the spleen, in the lymph nodes. And to understand how many effective T cells are in the body, you need to get the spleen, which, of course, no one will do to satisfy curiosity. Therefore, T-cell immunity cannot act as a marker. It is much easier to measure the level of antibodies, this is an integral indicator. It can always be determined by analyzing peripheral blood. But this does not mean that T-cell immunity does not play any role in protecting against coronavirus.
- In Russia, 60% was initially designated as the level of herd immunity, which would allow a return to normal life. Then, as the pandemic progressed and the vaccination process proceeded, that number began to rise. Is herd immunity really a cornerstone in defeating coronavirus and what percentage of vaccinated people is needed to do this?
- Herd immunity will indeed play a key role in defeating the coronavirus.
Here, no one refuses his words - although what you are saying now was not my voice.
But I also believe that intense herd immunity will form when people are immune either as a result of vaccination, or as a result of an illness, or the fact that some of the vaccinated get sick in a mild form - all this will play a role.
There is no other way.
The lethality of acute respiratory viral diseases, the pathogens of which enter the human population, is critically lower than the lethality of covid.
Even with the flu, especially if we take the swine flu, the lethality is only 0.04%.
And with COVID-19 - already 2%, if you divide the numbers provided by the WHO.
The difference in mortality is 50 times.
The first thing we will achieve as soon as the population is immune is to defeat the lethality.
With the victory over the incidence of COVID-19, the situation is more complicated, as well as with the overall incidence of acute respiratory viral infections.
In order not to get sick, it is necessary to constantly update the immune system - as is the case with the flu.
However, now the main goal of mankind is to obtain collective immunity and reduce mortality.
Reduce the burden on medical units, so that there are not so many hospitalizations so that doctors have time to cope and provide medical care.
So that the course of the infection is much easier than it is now.
- How safe is it to undergo revaccination if six months have passed after the first vaccination or illness, but the level of antibodies in a person remains high? Now this issue has acquired relevance due to the fact that the QR code of a patient who has recovered ceases to work after six months and a person must be vaccinated, despite the level of antibodies.
- Of course, this is always a personal story.
The very fact of an injection does not protect a person, you understand, it is necessary for a stable immunity to form.
And this will almost 100% protect you from the lethal outcome of the disease or from its severe course.
That is, from what should be feared in the case of a covid.
There are many reasons why people can develop both secondary and primary immunodeficiencies.
And if such a person is vaccinated with any vaccine, but immunity is not developed, of course, he will not be protected.
World Health Organization flag
AFP
© Fabrice Coffrini
I, as the deputy director of the Gamaleya Center, am not responsible for the regulation.
I can only tell you what has now come, for example, WHO, European Medical Association, FDA and CDC in the USA, Israel.
Nobody is now guided by the level of antibodies.
Everyone sees a decrease in the effectiveness of the vaccine, an increase in diseases six months after vaccination.
Nobody tests every person every three months to find out their antibody levels.
You see, on a national scale, certain measures are needed to protect the population - this is revaccination.
Revaccination is justified, it works, and not only in Russia, but also abroad.
Of course, you can dispute everything, say that each person needs to measure antibodies eight times and only then vaccinate.
If you come up with tools, a mechanism, how this can be done, I will listen to you with pleasure.
- How do you assess the scale of vaccination in Russia?
- Any rise in the incidence makes people think about the need to vaccinate.
Of course, we see an increase in vaccination - it always coincides with an increase in the incidence.
As soon as the incidence rate decreases, interest in vaccination also falls.
As I said, the case fatality rate from COVID-19 is fantastically higher than the case fatality rate from influenza.
And if people want to play roulette, looking at some acquaintances who have been ill easily, they are very much mistaken.
You need to face the truth and perform a very simple arithmetic operation.
Vaccination twenty, thirty times can reduce the likelihood of a person getting sick and dying.
Of course, in my opinion, you need to be vaccinated.
- Does the SARS-CoV-2 "delta" strain cause increased lethality?
- There is not a single publication in the world that "delta" increases the lethality in comparison with the "Wuhan" strain, we do not observe this.
The morbidity structure has changed.
For example, now more young children get sick than in the "wuhan", and much more.
There is a difference in transmissibility, this strain infects more people, the virus is secreted from the salivary glands in greater concentration.
There are other new properties - it better forms syncytia, cell fusion.
Thus, the virus spreads without even leaving the cell, where it can encounter antibodies.
The virus moves from membrane to membrane, or even forms a cell fusion.
The incubation period for the "delta" is no longer seven days, as it was with the "Wuhan" strain, but three to five.
This is a very short time, during such a time it is very difficult for the body to mobilize forces for protection if the immune system is not tense, but weakened (tense immunity is the level of the body's specific immunity to the causative agent of infection. -
RT
).
Medical workers and a patient in the intensive care unit of the COVID hospital, opened six months ago on the basis of the Regional Clinical Hospital No. 1 in Krasnodar
RIA News
© Vitaly Timkiv
The immune cell doubles every 18-24 hours.
In theory, in three days the body can strengthen its immune layer eight times - even less in real conditions.
When the incubation period is long, about 10-14 days, the immune layer has time to increase by about 16 thousand times, these are approximate figures.
But they allow us to understand what kind of handicap immunity has when the incubation period is long.
And for a short period, when the virus multiplies rapidly, it can overcome the immune system.
- Critics accuse the Russian president of not being vaccinated at gunpoint. Vladimir Putin said on a straight line that there was no point in this, if he said, then it was true. Do you think Russians generally need such a video?
-
It seems to me that this is a rather strange story, to be honest.
If you want to launch some kind of PR campaign at the expense of the president, this is fundamentally wrong.
And it means that with the understanding of the medical need to be vaccinated, something is wrong.
Not to mention the fact that you can always say that this is a vaccine, and inject something under the camera.
Therefore, it is unclear how such a video should motivate people to get vaccinated.
It is quite enough that the president said that he was grafted.
Re-checking the president's statements is definitely not my part.
And what upsets me is that very few people who work in the “red zone” listen to, see how many vaccinated and unvaccinated people get there.
They talk about it, but nobody hears them.
At the same time, there are “talking heads” with a huge number of subscribers who began to talk about virology without even having diplomas, having no relation to medicine.
But they have a huge audience, they captivate people with cheating ideas.
We need to popularize the vaccination process.
I am not saying that you need to be vaccinated with Sputnik, you need to be vaccinated with any vaccines registered in the country.
And you need to create a huge pool of vaccines so that people have a choice.
Trust does not arise out of the blue.
You see, we have no experience of mass vaccination of the adult population.
Since Soviet times, protection has been carried out through the vaccination of children.
Therefore, it would be naive to expect that the adult population will be vaccinated at once.
Rather, it is a long, arduous journey.
It is necessary to explain, to show by example, it is necessary for specialists to speak more.
RIA News
© Kirill Kallinikov
- Alexander Gintsburg said that an additional nasal vaccine vaccinated against the coronavirus will not carry the virus, how would you comment on this statement?
-
This is the goal we are striving for: to create not only systemic immunity, but also immunity at the gateway of infection.
This is necessary so that the infection does not have a handicap in front of immunity.
If the virus sat down on the mucous membranes, then it will take time until the immune cells that are in the spleen and lymph nodes are involved in the work.
And you can create an effective pool of immunocytes directly on the mucous membrane.
We think that if we form effective immunity where the infection enters the body, we can quickly get rid of it.
Create sterile immunity.
“The nasal vaccine is only being developed as an adjunct to the Sputnik
V
vaccination
, right?
- This is true.
But this is not an innovation, now there is, for example, a vaccine against poliomyelitis, when it is administered twice - first an inactivated vaccine, and then a live one, which causes barrier immunity on the mucous membranes.
This is a worldwide approved scheme, it works.
We want to reproduce it in the case of covid: first, create a good systemic immunity and also create a barrier immunity, which will be formed due to the tonsils located in the oropharyngeal ring.
-
In the future, will the nasal vaccine be enough to obtain
QR
codes?
Can it be offered in this case to anti-axers as an alternative?
- Yes, this is one of the tasks, as well as immunization of those who have already been vaccinated and those who have recovered.
As part of clinical research, we will understand how effective this approach is in protecting different cohorts of people.
I really hope that intranasal immunization will be enough.
But even if this is not the case, then there will be application for creating barrier immunity.
- When will this vaccine be ready for mass production?
“Perhaps as early as 2022, since this is a non-invasive method, we expect people to be recruited quickly for research.
Timing always depends on the recruitment of volunteers.
For example, the study may start in January 2022, the first and second phases will take several months.
In general, the forecast is optimistic.