- I wanted to talk about how it was with you, as a person who, during the spread of COVID in the USA, and mainly in New York, on his Facebook literally writing a book about how New York experienced COVID. How did it start?
- For me, it probably started with the same social networks, where suddenly in January they started discussing this strange virus. What is happening in China about the situation in Wuhan. There was quite a lot of information about this, everything is very controversial. Honestly, most of February, I thought it would be another Asian thing that will never reach us, or will come in the form of some sporadic cases that you need to know about, but which, most likely, will not become our problem .
“That's what most doctors thought, right?”
- Yes, we had some kind of training programs about COVID in the hospital, but all this was reminiscent of the situation with the Ebola virus in 2014. That you need to know about this, maybe it will concern you, but as a result of Ebola in New York there was exactly one case, and there were five in all the United States. It turned out quite wrong with COVID, and they started to understand that something was wrong somewhere in late February, when there were no tests, and more and more cases were recorded.
Then it was already clear that in a city like New York, this could not end well, in terms of the massive spread of infection. That is, we did not have any systems to prevent this.
- What quarantine measures were introduced in New York?
- Quarantine in New York was introduced on March 22, a lockdown was announced. Schools were closed on March 16th. Closed offices, restaurants. In principle, it was recommended to take the subway only to the necessary employees of hospitals and shops. They did everything so that the trains ceased to be a hotbed of distribution, but in the end they were filled anyway. No quarantine was observed. But they introduced him very late. The city declared quarantine only on March 22nd.
- How many ventilation devices were there in the city, when it became clear that they might not be enough?
“In New York itself, there were about a thousand resuscitation beds for eight million inhabitants.” When it all started in March, the speed of the emergence of new very difficult patients opened our eyes to the fact that these beds are most likely not enough.
- Why so little?
- They were enough. Even in the worst seasons, there were no problems during the H1N1 flu epidemic. It was in these epidemiological situations that New York did not need more resources.
- In the end, did you have enough devices?
- There were enough devices. In some places it was necessary to use operating apparatus, training. The state government, which had a reserve of ventilation devices, sent them to hospitals. Army apparatuses were sent from military bases. It was our, hospital, devices that were only enough for the first couple of weeks. If they didn’t help us, then before the peak we would definitely not be able to cope.
New York began an epidemic with an absolute lack of tests. At that time, 70% of the tests in the city were positive, because only patients whose suspected infection was close to 100% were tested. Hundreds of people a day were admitted to the city’s hospitals.
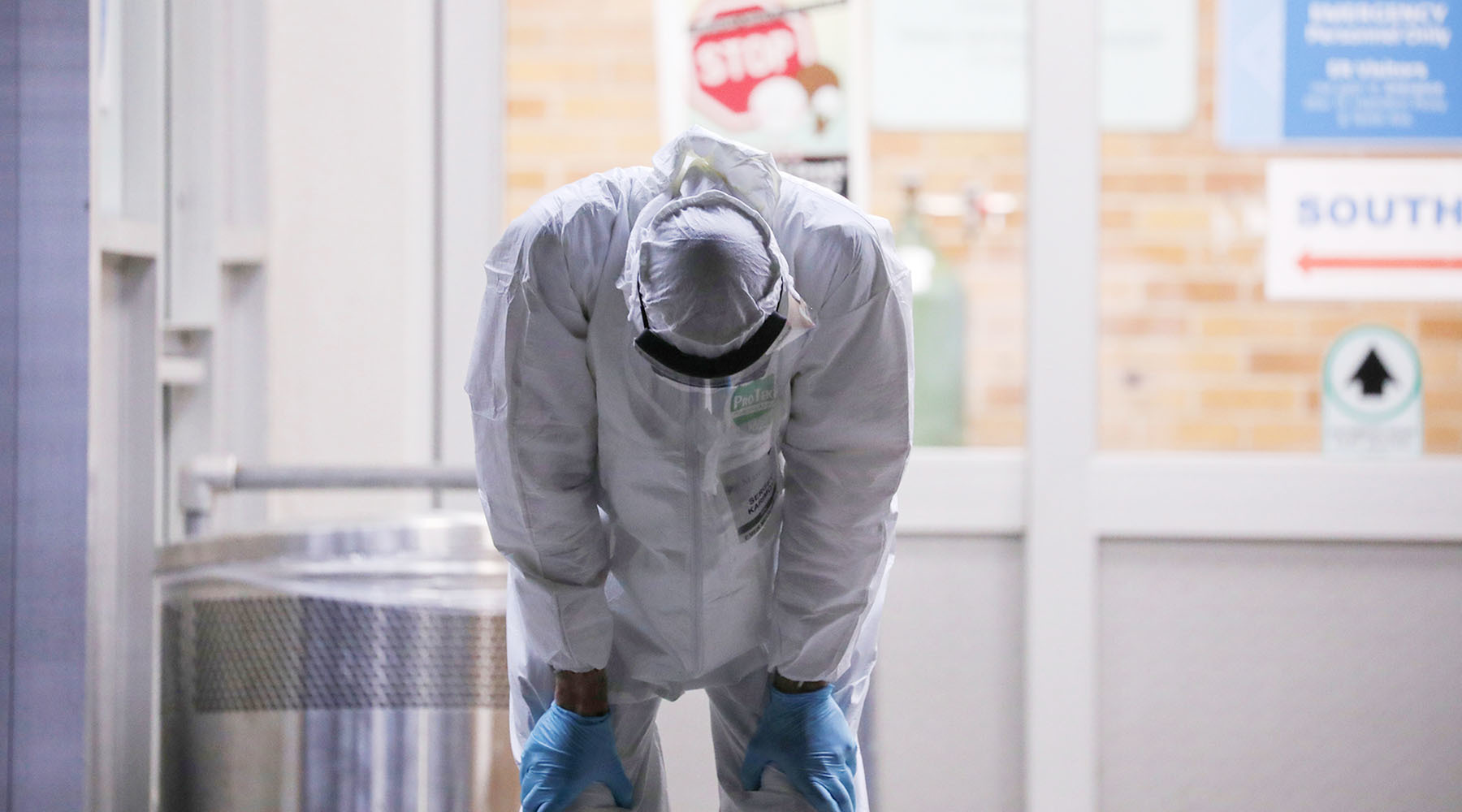
In a relatively small hospital with 400 beds, with 25-bed resuscitation, there were up to 15 transfers per day to IVL machines and hospitalization. At the peak of the epidemic in our hospital, there were about 500 patients, and 45 patients underwent mechanical ventilation. This is approximately two times the numbers with which we usually work.
- Reuters
- © Callaghan O'Hare
- Let’s talk with you as a resuscitator at all about mechanical ventilation. Attitude towards them changed as a whole by profession. We understood that there are situations when it is impossible not to put a person on mechanical ventilation, but we also understood that 80% would most likely die, and 20% would probably survive. To what extent was the use of such a large number of mechanical ventilation devices justified?
-Ventilation is a supportive therapy, it does not affect the disease itself. It simply gives the patient a chance to cope with the disease, supporting, in general, an idle organ. Unfortunately, mechanical ventilation is absolutely unnatural, this is not the process of breathing that nature has adapted to people. Therefore, mechanical ventilation has many problems and complications, the lungs are damaged during mechanical ventilation.
- And how are they damaged?
- Damage can be as a result of pressure, stretching of the alveoli, causing increased intrapulmonary inflammation. This is the so-called voli trauma, barotrauma - trauma with high pressure, which is required by the ventilator to deliver the gas mixture to the lungs.
“You say that you had 500 people at your peak.” How many of them during the pandemic lay on the ventilator, and how many of them survived as a percentage?
- It was the sharp ones that we had a maximum of 45 people. This is at the peak of the epidemic, somewhere in early April. Survival in the region is 45%, and about 30% came off mechanical ventilation. At the same time, there are still patients on ventilators. Some of them succeed, for some, unfortunately, there is a chance that they will need mechanical ventilation for many months, if not for life. As a result, there was a decent number of recoveries, that is, many patients went home after using mechanical ventilation. But, unfortunately, both disability and mortality were quite high.
- That is, we are talking about the fact that not just survival, but recovery on average in the region of 30%, right?
- Somewhere like that, yes. Because, of course, to survive, but to stay on the ventilator is a philosophical question, which is better.
- Let's talk about how the drugs were used. How did your idea of drugs change? Where did you start?
- We started like everyone with hydroxychloroquine. Still there is such a ping-pong, in what situation and to whom it is shown. We quickly realized that hydroxychloroquine did not help patients in the hospital. When respiratory failure began, even if patients did not need a ventilator, hydroxychloroquine did not improve the situation. And we quickly abandoned it, due to side effects - many patients had problems with cardiac arrhythmias.
- Inhibitor of interlekin-6 or "Actemra" its trade name. In Russia, it was often used literally as a miracle drug, everyone chased after it. How important was it for the removal of the cytokine storm and for maintaining the patient's life at the last crucial moment?
- It seems to me that it is in the resuscitation part of the course of the disease that this drug is ineffective. In any case, according to our observations inside the hospital. Its role is important precisely at the onset of a cytokine storm, with early symptoms of respiratory failure, before patients need serious oxygen support. If you give this drug to the right patients in time, you could avoid the situation when patients needed mechanical ventilation and, accordingly, their prognosis improved significantly.
“Who are the ordinary patients at your Brooklyn clinic?”
- This is a hospital for poor people with not very good insurance policies, for locals in this area of Brooklyn. This is a fairly poor area where high crime, a large number of people with many chronic diseases. Undoubtedly, such hospitals have suffered the most severe blow.
- Why, from your point of view, COVID was such a blow to the poor? Why have people with a little money, with poor insurance become the main segment of coronavirus infection?
- There are two factors. One social one is poor people who do not have resources, they cannot work remotely, they depend on their not very highly paid jobs. And this lack of money predisposes to the fact that they live in a more crowded environment. Plus a lower level of education, distrust of public resources. When they hear that they need to isolate themselves, they do not take it as seriously as others. The second part is medical. Although these people have insurance for the poor, most of them have neither the time nor the opportunity to get sick.
- Reuters
- © Caitlin Ochs
- Is such a heavy load on the medical system and such a large number of officially registered cases and deaths - is this such American statistics or is it really that America suffered a special blow?
- No one can understand. There is no evidence that another strain of the virus is working in other parts of the United States. Perhaps it is almost the full workload of the health system that predisposes to worse results. That is, mortality in Texas is lower because it is a vast territory, less crowded and a much more powerful healthcare system compared to New York.
Undoubtedly, the fact that we tested very little played a role. At the peak of the epidemic, we did not have enough tests, we tested only for symptoms ... People with some not-so-typical symptoms who might have coronavirus were refused to do the test simply because they do not have a temperature of 38 °.
I believe that tests were needed, and in much larger quantities than were available then in New York. We still do not know how many people are sick.
- American hospitals - did they close entirely, like Russian ones, under the coronavirus or departments?
- No, it was closed in our offices. But it struck me that almost all the other patients were missing. Yes, we have canceled planned operations and transferred all outpatient visits to telemedicine. But somewhere all the situations with which we deal every day have disappeared. And now it’s not entirely clear where all the pancreatitis, all thromboembolism, all bleeding have gone. There were very, very few of them. We had an intensive care unit for patients without COVID, and it was extremely rare for more than three to four people to appear in it. Despite the fact that our resuscitation is usually full.
- People with chronic diseases were simply afraid to go to the hospital, were afraid to get coronavirus there?
- Unfortunately, this is part of the situation, yes. Many people delayed their visit to the hospital as much as possible, trying with all their might to stay at home. Because it was really very scary.
“After five months of a pandemic in such a large city as New York, what did you begin to understand about coronavirus and such large-scale epidemics?”
- About coronavirus, I realized that the main thing is patience. Do not rush to immediately consider any new information that has appeared absolutely correct. Because knowledge changed over the course of weeks, if not days, and it was very strange. And also, I realized with great sadness that our health care system is not at all adapted for big shocks.
That is, it is a virus with a mortality rate in the region of 1%. In theory, how can such a rich, so medically advanced country like America simply fall to its knees before such an illness?
But we still do not understand what to do next. We are in endless quarantine, we are afraid to leave it, and this is true, because we realized that our health care system, which can treat some completely crazy things, is just in this situation, in a situation of a massive number of infected people, it’s not very adapted .
- Why is this happening? Because the American health care system is designed specifically for the enormous costs of insurance medicine or the patient itself and does not pay attention to some, as it seems to her, husks - ARVI, people with low incomes?
- The economic part is present in this situation. Indeed, it is more profitable to perform planned operations, more profitable to treat for rare expensive diseases than to treat patients with some massive, but not such an interesting problem. Unfortunately, we just lived for many years in a fairly comfortable world that changed little, there were few such medical shocks.
We kind of knew everything, and roughly imagined what we were going to deal with, but when faced with reality, it turned out that it was not like that at all. And so many were shocked. Many of my colleagues, including those who were here during the September 11 attacks and during the H1N1 epidemic, were all unpleasantly surprised by the situation with coronavirus. It was something unprecedented even for them.
“Do we understand what to do when the next big pandemic happens?”
- Undoubtedly, we have learned some lessons. Now, in a situation of a respiratory virus, we understood how to work with isolation, how to work with contacts, how to accumulate protective equipment, how to deal with a shortage of ventilation devices, if any. But we don’t know exactly what will be the next pathogen.
- What do you think: treatment or vaccination?
- So far we can only dream of a vaccine. Not everyone will want to test for themselves some raw, untested vaccine. Of course, I would like some kind of antiviral treatment, except for the use of remdesivir - wildly expensive, not available in oral form, but still, something that works at an early stage, and even better - to find some kind of working post-exposure prophylaxis.
So far, unfortunately, most antiviral drugs fail in this situation. We still don’t know what works at the very beginning of the disease, before the patient’s condition worsens so much that all kinds of resources are needed to save a life.
- That is, there is no treatment yet. And, if I understand correctly, it is unlikely to appear in the next six months.
- I think yes. The only thing that now shows at least some effectiveness is remdesivir in certain patients, if given on time. Again, price, inconvenience, side effects - all this is present. There are no other antiviral drugs. What we still do not know is how to predict which of the patients, having become infected with the virus, will go to the hospital, and who will feel bad. That is, we still do not have clear criteria for how to predict a severe course.
Somewhere by mid-May, all patients with a severe course of coronavirus practically disappeared. We closed additional resuscitation. Now, in general, we are working as usual. I work in several New York hospitals, and the situation is the same everywhere.
- That is, there is practically no heavy current. Seasonal virus?
- Actually a seasonal virus, yes. Now somewhere in the hospital there is a patient with coronavirus, but they are not in intensive care, and they do not get practically. At the same time, the seasonal virus has passed in New York, while in Minnesota, on the contrary, now there is an increase in cases. So far, very unpredictable and very strange epidemiology. But in New York, indeed, everything went exactly on the principle of a very fast exponent and a very sharp decline.